Describing rashes A rash is a change in the colour or texture of the skin and as such reflects the nature and pattern of a collection of individual lesions. A major consideration in dermatological assessment is to determine the specific patterns of such rashes and their specific characteristics as an aid to diagnosis. Some of the dimensions of skin assessment are specified in Table 3.3. These include site, colour, acuity, surface features and type of lesion. | | | | | | Table 3.3 A framework for skin assessment and lesion description. | | 1. Site
2. Erythematous, i.e. reddened skin (blanches on pressure) or non-erythematous
3. Acute (<2 weeks duration) or chronic (>2 weeks duration)
4. Surface features
a. Normal/smooth (i.e. same as surrounding skin)
b. Scaly
c. Hyperkeratotic
d. Warty
e. Crust
f. Exudate
g. Excoriated 5. Type of lesion
a. Flat: macules and patches
b. Raised: papules, plaques and nodules
c. Fluid-filled: vesicles, bullae and pustules
d. Surface broken: erosions, ulcers and fissures If non-erythematous describe the
6. Colour
a. Due to blood: pink, purple, mauve
b. Due to pigment: brown, black and blue
c. Due to lack of blood/pigment: white
d. Other colours: yellow, orange, grey |
| | | |
Source: Based on Ashton and Leppard (2005). | |
|
Owing to the wide-ranging nature of lesions, it is helpful to understand their different types. Therefore, specific definitions and clinical examples of particular surface features and lesions are now summarised in Table 3.4. | | | | | | Table 3.4 Types and definitions: Surface features and lesions. | | Types of lesion | | | | Normal | Smooth, the absence of other surface features | | | Scaly | Excess dead epidermal scales produced by shedding from the stratum corneum or abnormal keratinisation (e.g. erythrodermic psoriasis) | | | Hyperkeratotic | Increased keratinisation (cornification) of the epidermis, which appears clinically as thickened and rough skin or mucous membrane (e.g. foot psoriasis) | | | Warty | A wart-like lesion consisting of finger-like projections (e.g. filiform wart) | | | Crust | Dried exudate (comprised of dried serum, bacteria and possibly blood, mixed with epidermal debris – e.g. impetigo) | | | Excoriated | A superficial linear erosion caused by excessive scratching (e.g. atopic eczema) | | | Exudate | A leakage of fluid from blood vessels into nearby tissue (e.g. acute eczema) | | | Flat: macule | A flat lesion circumscribed area of altered skin colour <1 cm in diameter (e.g. vitiligo, solar lentigo) | | | Flat: patch | A flat lesion >1 cm in diameter (e.g. port wine stain) | | | Raised: papule | A raised lesion <1 cm in diameter (e.g. compound naevus) | | | Raised: plaque | A slightly raised flat-topped lesion >1 cm in diameter of surface skin (e.g. plaque psoriasis, pityriasis rosea) | | | Raised: nodule | A solid palpable mass that is larger than 1 cm whose greater part lies beneath the skin (e.g. erythema nodosum, basal cell carcinoma) | | | Fluid-filled: vesicle | A small lesion <5 mm in diameter, fluid-containing elevation (e.g. herpes simplex, eczema herpeticum) | | | Fluid-filled: bullae | A lesion >5 mm in diameter, fluid-containing elevation (e.g. bullous pemphigoid) | | | Fluid-filled: pustule | A lesion <1 cm filled with pus (e.g. acne vulgaris) | | | Due to broken surface: ulcer | Loss of epidermis and dermis (e.g. ducibitus [pressure] ulcer) | | | Due to broken surface: erosion | Loss of epidermis only (e.g. intertrigo - a rash in body folds) | | | Due to broken surface: fissure | Linear split in skin: foot psoriasis (e.g. a heel fissure) | | | Colour: due to blood | Petechia (pin head size) (e.g. Meningococcal disease – that do not disappear when pressure if applied) – they are purpuric lesions up to 2 mm across; Purpura (<2.5 mm): red, purple or orange/brown colour due to blood leaking from blood vessels (does not blanche under pressure) (e.g. drug eruption, allergic vasculitis); Haematoma (bruise); Telangiectasia: spider-like capillaries (e.g. due to chronic treatment with topical corticosteroids) | | | Colour: due to pigment | May be due to increase in melanin pigment following epidermal inflammation (e.g. lichen planus) | | | Colour: due to lack of blood/pigment | Depigmentation: complete loss of melanin (e.g. vitiligo) Hypopigmentation: partial melanin loss due to epidermal inflammation (e.g. eczema) | | | Colour: other | Yellow (e.g. xanthelasma) |
| | | | | |
|
A useful distinction is also made of primary and secondary lesions. Primary lesions are caused directly by the disease process; this includes macules, papules, nodules, plaques, wheals, vesicles, bulla, pustules and cysts (Figures 3.3–3.8). Secondary lesions refer to the consequences of the disease process; these include scale, crust, fissures, lichenification, erosion, ulcers, excoriation, scar and atrophy (Johannsen, 1998). Further details of physical signs in dermatology, with excellent illustrative photographs, can be found in Lawrence and Cox (2002). Many skin diseases have a classic distribution which aids diagnosis; this is illustrated in Figure 3.9.  | | Figure 3.3 Macule. (Source: Reprinted from Graham - Brown and Burns, 2006.) |
| |  | | Figure 3.4 Plaque. (Source: Reprinted from Graham - Brown and Burns, 2006.) |
|
 | | Figure 3.5 Papule. (Source: Reprinted from Graham - Brown and Burns, 2006.) |
| |  | | Figure 3.6 Vesicle. (Source: Reprinted from Graham - Brown and Burns, 2006.) |
|
 | | Figure 3.7 Bullae. (Source: Reprinted from Graham-Brown and Burns, 2006.) |
| |  | | Figure 3.8 Nodule. (Source: Reprinted from Graham-Brown and Burns, 2006.) |
|
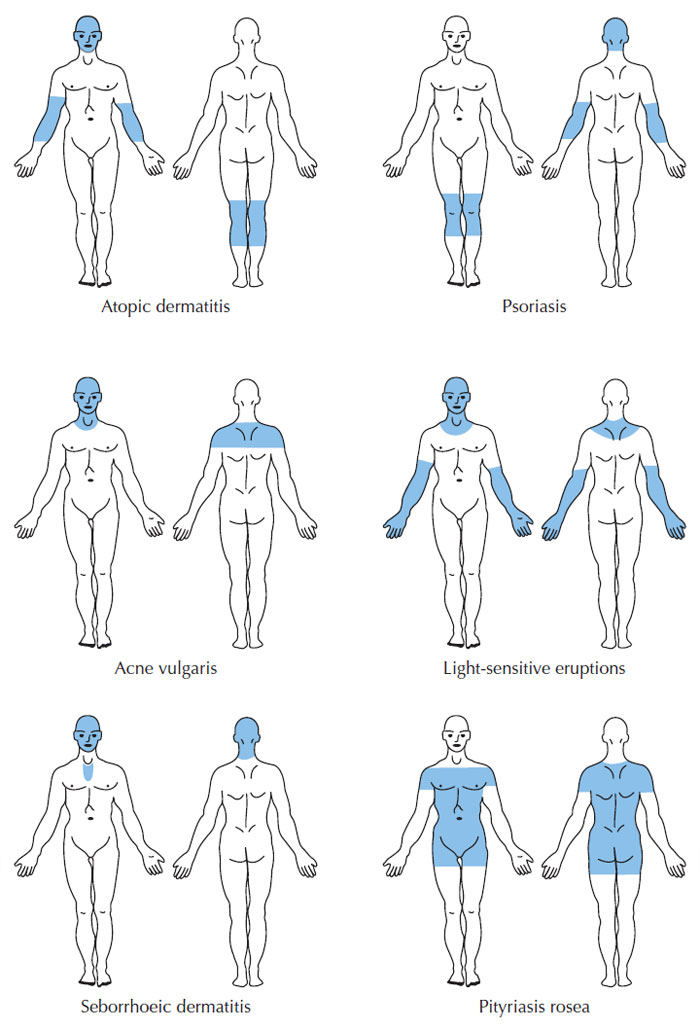 | | Figure 3.9 Classic lesion distribution in common skin disorders (Mackie, 2003). |
|