|
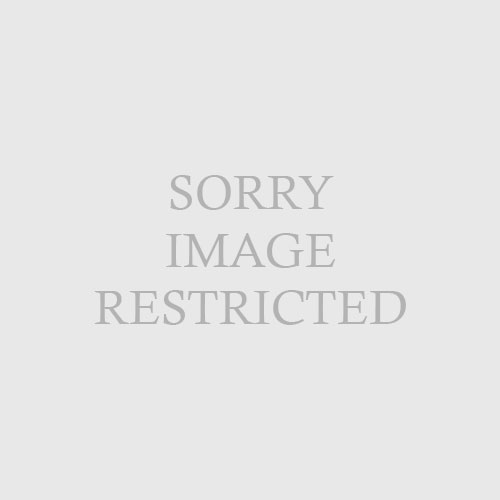
| Fig. 32.9 Disseminated coccidioidomycosis. Discrete verrucous papules, plaques, and nodules. (Courtesy of James E. Fitzpatrick, MD.) |
Primary pulmonary infection is asymptomatic in 50% of patients. In 40%, patients present with a mild flulike illness or pneumonia. Erythema nodosum is present in 5% of patients with acute coccidioidomycosis. Hematogenous dissemination occurs in 1% to 5% of patients. Risk factors for dissemination and fatal disease include male sex, pregnancy, immunocompromised status, and race (in order of decreasing risk by race: Filipino, black, and white). Among immunosuppressed patients, lymphocytopenia correlates closely with dissemination. Coccidioidomycosis is considered an AIDS-defining illness. The most common sites of extrapulmonary disease include the skin, lymph nodes, bones/joints, and central nervous system (meninges). Cutaneous lesions of disseminated coccidioidomycosis are protean. Warty papules, plaques, or nodules are the most characteristic (Fig. 32-9). Cellulitis, abscesses, and draining sinus tracts also may occur. Rarely, cutaneous lesions can be from primary cutaneous inoculation. Erythema nodosum is the most common reactive manifestation of coccidioidomycosis and indicates a robust cell-mediated immune response. Other reactive patterns include generalized morbilliform, papular, targetoid or urticarial exanthem, interstitial granulomatous dermatitis, and Sweet syndrome.
DiCaudo DJ: Coccidioidomycosis: a review and update,
J Am Acad Dermatol 55(6):929–942, 2009.